INTRODUCTION
Hemophilia is a bleeding disorder that slows the blood clotting process. People with this condition experience prolonged bleeding or oozing following an injury, surgery, or having a tooth pulled. In severe cases of hemophilia, continuous bleeding occurs after minor trauma or even in the absence of injury (spontaneous bleeding). Serious complications can result from bleeding into the joints, muscles, brain, or other internal organs. Milder forms of hemophilia do not necessarily involve spontaneous bleeding, and the condition may not become apparent until abnormal bleeding occurs following surgery or a serious injury.
TYPES OF HEMOPHILIA
The two main types of hemophilia are A and B, according to the National Hemophilia Foundation. A third, rarer form of the disease is called hemophilia C. Each type is directly related to a specific factor, namely, hemophilia A is a Factor VIII deficiency, hemophilia B is a Factor IX deficiency and hemophilia C is a Factor XI deficiency.
Hemophilia type A
Hemophilia A is a genetic disorder caused by missing or defective Factor VIII protein. It is inherited, but in about one-third of known cases it is caused by a spontaneous genetic mutation.
The blood disorder affects all ethnic groups equally. More than half of all people with hemophilia A have a severe form of the disease.
Hemophilia A is carried by the X chromosome. It is inherited in an X-linked recessive manner. As such, two hemophilia-carrying X chromosomes must be inherited for the disease to be active in women, but only in one X chromosome for men.
A female inherits two XX chromosomes, one from her mother and one from her father (XX). A male inherits an X chromosome and a Y chromosome from her father (XY). This means that if a son inherits an X chromosome from his mother who carries hemophilia, he will have hemophilia. But because women receive two X chromosomes, only if both parents carry the defective gene can they develop the disease.
Hemophilia A has three stages: mild, moderate and severe, depending on the ratio of Factor VIII clotting protein in the blood. Mild hemophilia 6-49 percent, moderate hemophilia is 1-5 percent, and severe is less than 1 percent.
People with hemophilia A bleed longer than others, internally or externally. Those with mild hemophilia A generally bleed only after serious injury, trauma or surgery. Often, the disease is diagnosed after one of these situations due to prolonged bleeding, and the first episode may occur only in adulthood. Women often experience heavy menstrual periods and can hemorrhage after giving birth.
Moderate hemophilia patients tend to have more frequent bleeding episodes after less important injuries, or even spontaneously. In severe cases, bleeding may occur spontaneously in the joints and muscles.
Hemophilia A should be diagnosed and treated at a specialized hemophilia center. Tests that evaluate clotting time and a patient’s ability to form a clot may be ordered. A clotting factor test, called an assay, will determine the type of hemophilia and its severity.
The main treatment for hemophilia A is concentrated Factor VIII product, which is administered intravenously.
Patients with severe hemophilia may be given a routine treatment regimen called prophylaxis to maintain enough clotting factor in their bloodstream to prevent bleeds.
Hemophilia type B
Hemophilia B is a genetic disorder caused by missing or defective Factor IX clotting protein. It is also inherited, and just like hemophilia A, it can be caused by a spontaneous genetic mutation in one-third of the cases. This type of hemophilia also affects all ethnic groups equally, but it is about four times as rare as hemophilia A.
Hemophilia B is also carried in the X chromosome, in an X-linked recessive manner, meaning that two hemophilia-carrying X chromosomes must be inherited for the disease to be active in women, but only in one X chromosome in men.
Females inherit two XX chromosomes, one from their mother and one from their father (XX). Males inherit an X chromosome and a Y chromosome from their father (XY). This means that is a son inherits an X chromosome from his mother that has carries hemophilia, he will have hemophilia. But because women receive two X chromosomes, it’s only if the two carry the defective gene, that they develop the disease.
Severity levels are the same as hemophilia A, as well as symptoms.
Like hemophilia A, hemophilia B should be diagnosed at a specialized medical facility. Tests that evaluate clotting time and a patient’s ability to form a clot may be ordered. A clotting factor test, called an assay, will determine the type of hemophilia and its severity.
In hemophilia B, the most common treatment is the administration of concentrated Factor IX, administered intravenously. Severe cases of hemophilia B will also be on prophylaxis treatment, to maintain Factor IX clotting factor.
Hemophilia type C
Hemophilia C is a genetic disorder caused by missing or defective Factor XI clotting protein. The disease was first recognized in 1953 in patients who experienced severe bleeding after dental extractions.
The incidence of hemophilia C is estimated at one in every 100,000 people in the general population. In Israel, Factor XI deficiency occurs in up to 8 percent of Ashkenazi Jews due to intermarriage. This is because a Factor XI deficiency is inherited in an autosomal recessive pattern, meaning both parents must carry the gene to pass it on to their children. Unlike hemophilia A and B, men and women are affected equally.
Factor XI plays an important role in the clotting cascade, which leads to clotting. It helps generate more thrombin, a protein that converts fibrinogen to fibrin, which traps platelets and helps hold a clot in place.
Unlike hemophilia A and B, symptoms don’t correlate with Factor XI levels in the blood. People with lower levels may bleed less than those with higher levels of Factor XI. Patients often experience nosebleeds or soft tissue bleeds, as well as hemorrhaging after tooth extraction.
Many women may not know they’re deficient in Factor XI until they experience menorrhagia (heavy menstrual periods) or postpartum bleeding. In hemophilia C, joint and muscle bleeds are uncommon.
To diagnose hemophilia C, doctors will order a bleeding time test, platelet function tests, and prothrombin time (PT) and activated partial thromboplastin time (aPTT) tests.
Factor XI concentrates are unavailable in the United States as yet, so doctors normally treat hemophilia C with fresh frozen plasma. But because Factor XI is not concentrated in this treatment, large amounts may be necessary, which can lead to blood clots. This treatment must be administered carefully.
Fibrin glue is also used to maintain clots after mouth bleeds. When combined with fresh frozen plasma, it arrests bleeding after circumcision and hernia repair. Antifibrinolytics are used to control nose bleeds or bleeding after tooth extraction.
SYMPTOMS
The major symptom is bleeding, either prolonged external bleeding or bruising after minor trauma or for no apparent reason. Symptoms vary depending on whether the patient has the mild, moderate, or severe form of the disorder:
- In severe hemophilia, unprovoked (spontaneous) bleeding episodes occur often.
- In moderate hemophilia, prolonged bleeding tends to occur after a more significant injury.
- In mild hemophilia, a patient might have unusual bleeding, but only after a major injury, surgery, or trauma.
People with hemophilia may have any type of internal bleeding, but most often it occurs in the muscles and joints, such as the elbows, knees, hips, shoulders and ankles. There may be no pain at first, but if the bleeding continues, the joint may become hot to the touch, swollen, and painful to move.
Repeated bleeding into the joints and muscles over time may cause permanent damage, such as joint deformity and reduced mobility.
Bleeding in the brain is a very serious problem for those with severe hemophilia. It may be life-threatening. Get medical help immediately if you have signs of bleeding, such as:
- Changes in behavior.
- Excessive sleepiness.
- Headache that will not go away.
- Neck pain.
- Double vision.
- Vomiting.
- Convulsions or seizures.
CAUSES
When you bleed, your body normally pools blood cells together to form a clot to stop the bleeding. The clotting process is encouraged by certain blood particles. Hemophilia occurs when you have a deficiency in one of these clotting factors.
There are several types of hemophilia, and most forms are inherited. However, about 30% of people with hemophilia have no family history of the disorder. In these people, an unexpected change occurs in one of the genes associated with hemophilia.
Acquired hemophilia is a rare variety of the condition that occurs when a person's immune system attacks clotting factors in the blood. It can be associated with:
· Pregnancy
· Autoimmune conditions
· Cancer
· Multiple sclerosis
Hemophilia inheritance
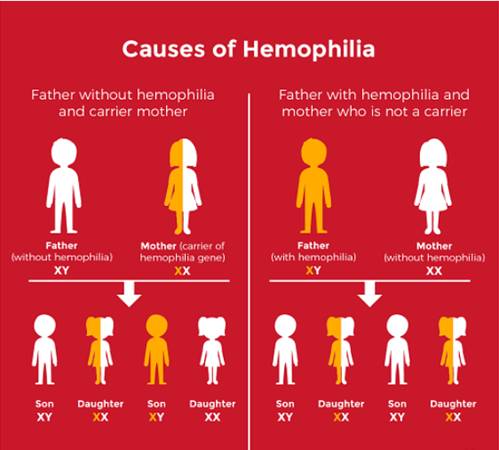
In the most common types of hemophilia, the faulty gene is located on the X chromosome. Everyone has two sex chromosomes, one from each parent. A female inherits an X chromosome from her mother and an X chromosome from her father. A male inherits an X chromosome from his mother and a Y chromosome from his father.
This means that hemophilia almost always occurs in boys and is passed from mother to son through one of the mother's genes. Most women with the defective gene are simply carriers and experience no signs or symptoms of hemophilia. But some carriers can experience bleeding symptoms if their clotting factors are moderately decreased.
RISK
The biggest risk factor for hemophilia is to have family members who also have the disorder.
DIAGNOSIS
The majority of patients with hemophilia have a known family history of the condition. However, about one-third of cases occur in the absence of a known family history. Most of these cases without a family history arise due to a spontaneous mutation in the affected gene. Other cases may be due to the affected gene being passed through a long line of female carriers.
If there is no known family history of hemophilia, a series of blood tests can identify which part or protein factor of the blood clotting mechanism is defective if an individual has abnormal bleeding episodes.
The platelet (a blood particle essential for the clotting process) count and bleeding time test should be measured as well as two indices of blood clotting, the prothrombin time (PT) and activated partial thromboplastin time (aPTT). A normal platelet count, normal PT, and a prolonged aPTT are characteristic of hemophilia A and hemophilia B. Specific tests for the blood clotting factors can then be performed to measure factor VII or factor IX levels and confirm the diagnosis.
Genetic testing to identify and characterize the specific mutations responsible for hemophilia is also available in specialized laboratories.
TREATMENT
Treatment depends on the type and severity of the disorder. It consists of replacement therapy, in which human plasma concentrates or recombinant (produced from DNA) forms of the clotting factors VIII or IX are given to replace the blood clotting factors that are missing or deficient.
- Blood factor concentrates are made from donated human blood that has been treated and screened to reduce the risk of transmitting infectious diseases, such as hepatitis and HIV.
- Recombinant clotting factors, which are made in the laboratory and not from human blood, are commonly used today.
- Recombinant FVIII and FIX products, modified to survive longer in the circulation, are now available. They required less frequent dosing for prophylaxis or prevention of bleeding.
- Newer non-factor products are also being developed for prophylactic use in hemophilia. These have the advantage of much less frequent administration, and in some cases do not require intravenous administration.
During replacement therapy, the clotting factors are injected or infused (dripped) into a patient’s vein in the arm or a port in the chest. Usually, people with mild or moderate hemophilia do not need replacement therapy unless they are going to have surgery.
- In cases of severe hemophilia, treatment may be given to stop bleeding when it occurs. Patients who have frequent bleeding episodes may be candidates for prophylactic factor infusions. These are given two or three times per week to prevent bleeding from occurring.
- Some people with the mild or moderate form of hemophilia type A can be treated with desmopressin (DDAVP®), a synthetic (man-made) hormone that helps to stimulate the release of factor VIII and another blood factor that carries and binds to it. Sometimes desmopressin is given as a preventive measure before a person with hemophilia has dental work or some other minor surgical procedure. Desmopressin does not work for people with type B hemophilia or severe hemophilia A.
- Aminocaproic acid or tranexamic acid are agents that prevent clots from breaking down (“antifibrinolytics”). They may be used as an added therapy to treat nosebleeds or bleeding from having a tooth removed.
The only absolute cure for hemophilia is a liver transplant. However, much progress is being made in finding a genetic cure for persons with hemophilia.